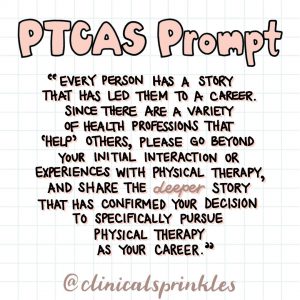
PTCAS Personal Statement Prompt 2021-2022
If you're applying for a Doctor of Physical Therapy (DPT) Program for the 2021-2022 cycle, you're in the right place.
This year's prompt matches last year's prompt which is:
Every person has a story that has led them to a career. Since there are a variety of health professions that “help” others, please go beyond your initial interaction or experience with physical therapy, and share the deeper story that has confirmed your decision to specifically pursue physical therapy as your career.
This is an elaborate way of asking... Why physical therapy? Why PT above all other health professions?
If your answer is simply, "because I want to help people," I'm going to be the one to tell you that you're going to need to dig a lot deeper than that. The prompt literally asks for a deeper story.
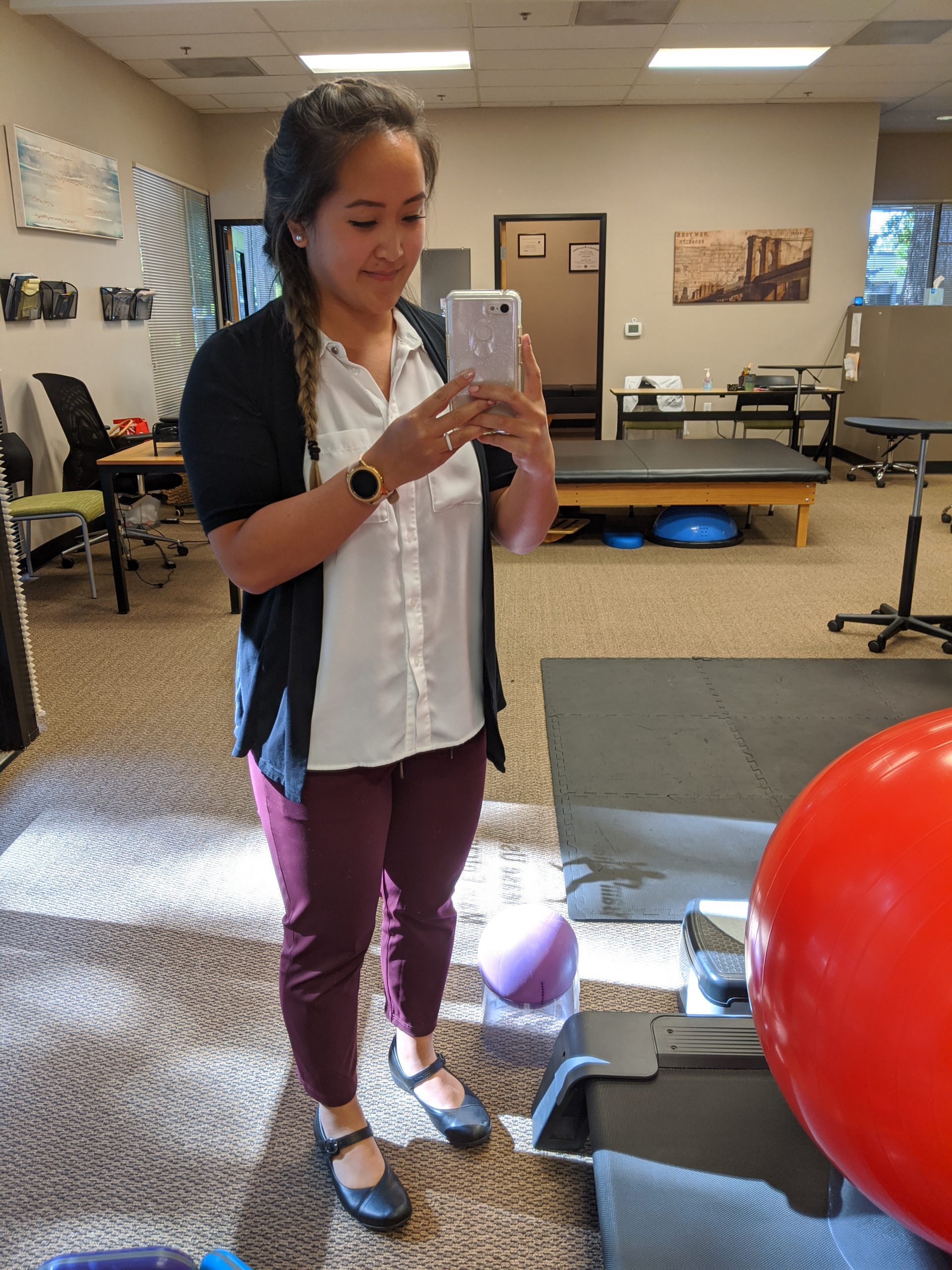
You don't have to have been a patient in PT to want to apply to PT school. I hadn't been a patient myself before I applied to school. Through observation hours and more, I found my calling in PT. I share my "PT why" in my personal statement for the 2013-2014 cycle here.
If you're finding yourself scrambled on how to write your essay or even how to start, a coaching call may be the best option for you. I've helped several pre-PT, pre-OT, pre-PA, and pre-med, students with their personal statements, and they've successfully been accepted. I specialize in finding the deeper WHY and making sure the writer is showing, not telling.
If you've already have what you think is a close-to-final draft, I also provide consults to go over the essay with an unbiased view and help you bring in an emotional touch to your story to captivate the reader. I had a less than ideal application and I believe my personal statement helped me stand out. Read more about my less-than-ideal application here.
Good luck to all of those applying! And follow @clinicalsprinkles on Instagram for more application tips and learning about the life of an outpatient ortho PT.

 𝗕𝗘 𝗣𝗥𝗘𝗣𝗔𝗥𝗘𝗗
𝗕𝗘 𝗣𝗥𝗘𝗣𝗔𝗥𝗘𝗗





 I lacked confidence for the first year out of school and had a lot of anxious feelings the first six months after graduating. Was I helping my patients? Will they get better? Would they be better off with another PT?
I lacked confidence for the first year out of school and had a lot of anxious feelings the first six months after graduating. Was I helping my patients? Will they get better? Would they be better off with another PT?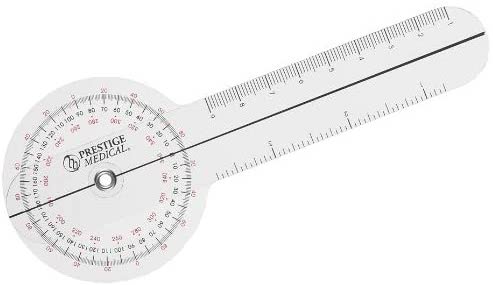






 I currently work in outpatient ortho but this clinical rotation alone made me love PT in a skilled nursing facility as well. Maybe it was the whole rehab team that made this rotation and setting so special. On my first day, the staff teased me that I’m in for a special treat at lunch. I was nervous because they wouldn’t tell me what it was. To my surprise, the “treat” was their ongoing tradition to play hacky-sack during lunch. If you’ve been following my page for a while, you’ll know I have very little to no coordination. We never missed a day.
I currently work in outpatient ortho but this clinical rotation alone made me love PT in a skilled nursing facility as well. Maybe it was the whole rehab team that made this rotation and setting so special. On my first day, the staff teased me that I’m in for a special treat at lunch. I was nervous because they wouldn’t tell me what it was. To my surprise, the “treat” was their ongoing tradition to play hacky-sack during lunch. If you’ve been following my page for a while, you’ll know I have very little to no coordination. We never missed a day.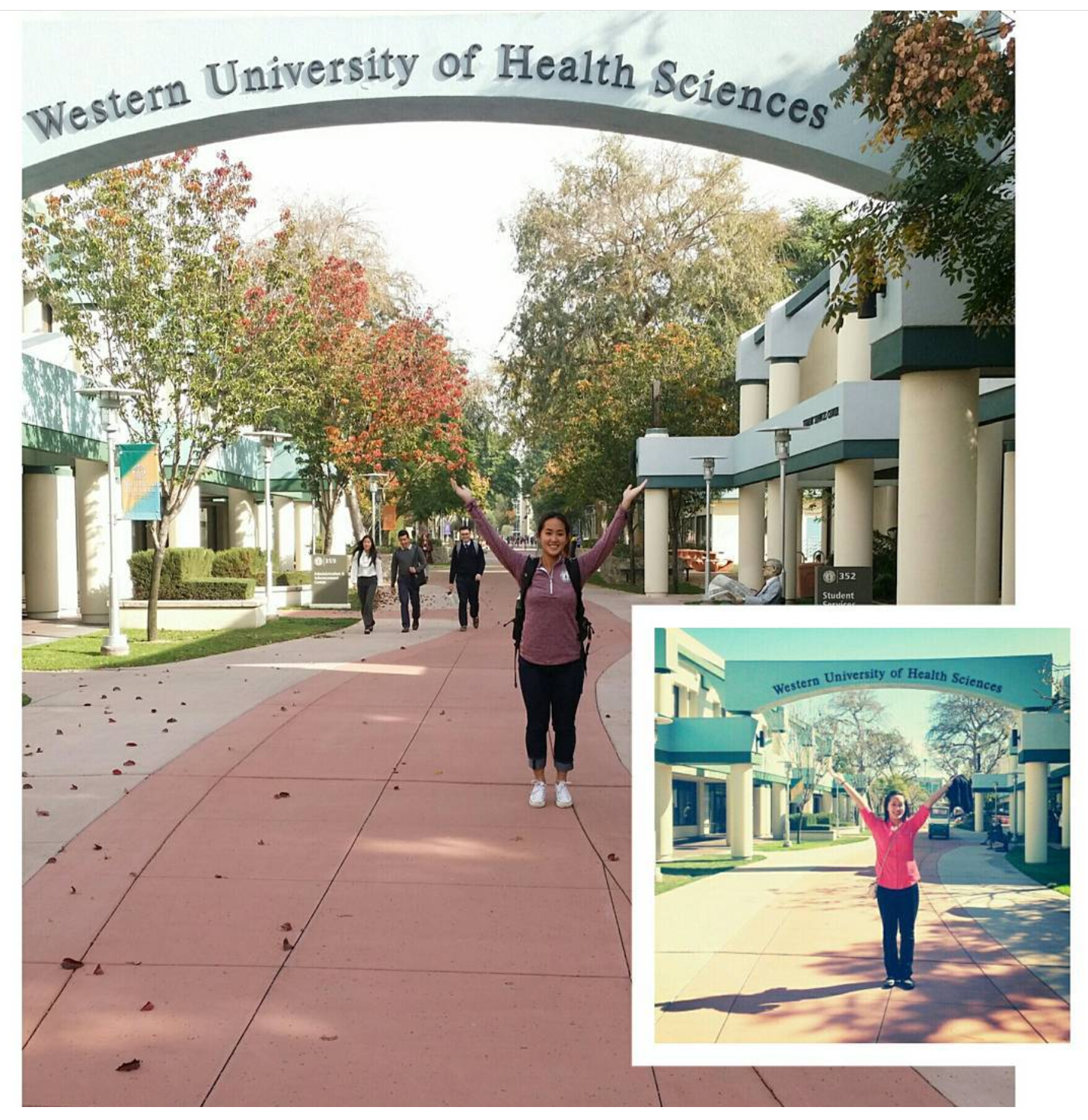 I was fortunate to have my last two affiliations back near home in Oregon. My PT program was located in Pomona, CA. My last day in Cali was a final and a celebration with my class (there may have been a party bus) and when I got home, I woke my husband up (around 3 am), took a 30-minute nap while he showered and we hit the road. 18-hour drive back to Oregon.
I was fortunate to have my last two affiliations back near home in Oregon. My PT program was located in Pomona, CA. My last day in Cali was a final and a celebration with my class (there may have been a party bus) and when I got home, I woke my husband up (around 3 am), took a 30-minute nap while he showered and we hit the road. 18-hour drive back to Oregon.