Inspirations for Clinical Sprinkles
 I started my Instagram page over a year ago and was sharing my experiences with learning within the orthopedic residency and it was a mix of PT and fitness.
I started my Instagram page over a year ago and was sharing my experiences with learning within the orthopedic residency and it was a mix of PT and fitness.
Not until the Coronavirus did I really buckle down and create a business out of this page to change my IG handle to @clinicalsprinkles.
The page has grown into a platform where I help pre-PTs, student PTs, and current DPTs to develop professionally and clinically.
As a pre-PT, I had a less than ideal application with a relatively low GPA and average GRE scores. My application was enhanced by my extracurriculars and personal statement. Hear my personal statement here. I have helped many others with their essays before creating this page and they have locked in their placement into their dream schools. I realized I have a talent for building an emotional connection with a reader and want to share this with others. Find out more about how I help with this here.
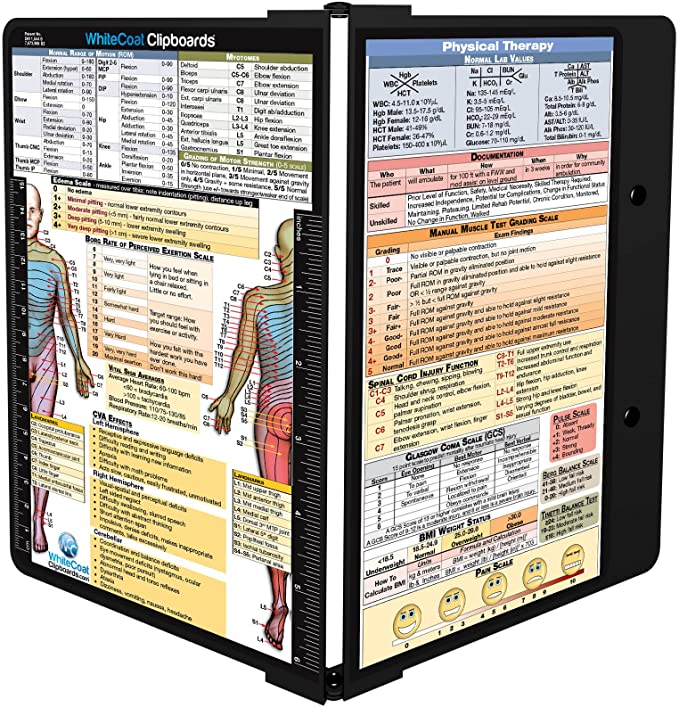
For student PTs, I have created resources to help prepare for clinical and what to look for in a job. I share my tips on my YouTube page and also on my website.
Throughout my 4 years of practicing as an outpatient PT,
I found myself saying, “wow, I wish I would have known about this sooner”
multiple times. So I’m sharing “clinical sprinkles” with you to help you stumble less and make progress with your patients sooner. Also, become a better communicator and listener. Both of which are essential skills for this job.
My inspirations come from my experience and my passion for helping others. I want to help others grow within this amazing profession and help build each other up.

 I lacked confidence for the first year out of school and had a lot of anxious feelings the first six months after graduating. Was I helping my patients? Will they get better? Would they be better off with another PT?
I lacked confidence for the first year out of school and had a lot of anxious feelings the first six months after graduating. Was I helping my patients? Will they get better? Would they be better off with another PT? If you’re pre-physical therapy, most schools require you to complete a certain number of observation hours before you apply. If you’re a student observer, these tips are for you.
If you’re pre-physical therapy, most schools require you to complete a certain number of observation hours before you apply. If you’re a student observer, these tips are for you. Patients need to be active players in their recovery as well. We know this as PTs, but we need to teach our patients this concept.
Patients need to be active players in their recovery as well. We know this as PTs, but we need to teach our patients this concept.






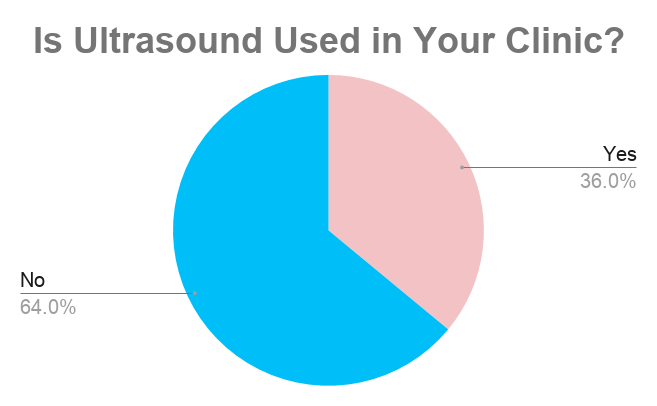
 I practice physical therapy in an outpatient orthopedics clinic. It’s been almost two weeks working at a new one and I’ve found many differences. Differences that make me feel like I have to change the way I practice. Here are some of the differences and what/how I’ve changed.
I practice physical therapy in an outpatient orthopedics clinic. It’s been almost two weeks working at a new one and I’ve found many differences. Differences that make me feel like I have to change the way I practice. Here are some of the differences and what/how I’ve changed. I currently work in outpatient ortho but this clinical rotation alone made me love PT in a skilled nursing facility as well. Maybe it was the whole rehab team that made this rotation and setting so special. On my first day, the staff teased me that I’m in for a special treat at lunch. I was nervous because they wouldn’t tell me what it was. To my surprise, the “treat” was their ongoing tradition to play hacky-sack during lunch. If you’ve been following my page for a while, you’ll know I have very little to no coordination. We never missed a day.
I currently work in outpatient ortho but this clinical rotation alone made me love PT in a skilled nursing facility as well. Maybe it was the whole rehab team that made this rotation and setting so special. On my first day, the staff teased me that I’m in for a special treat at lunch. I was nervous because they wouldn’t tell me what it was. To my surprise, the “treat” was their ongoing tradition to play hacky-sack during lunch. If you’ve been following my page for a while, you’ll know I have very little to no coordination. We never missed a day.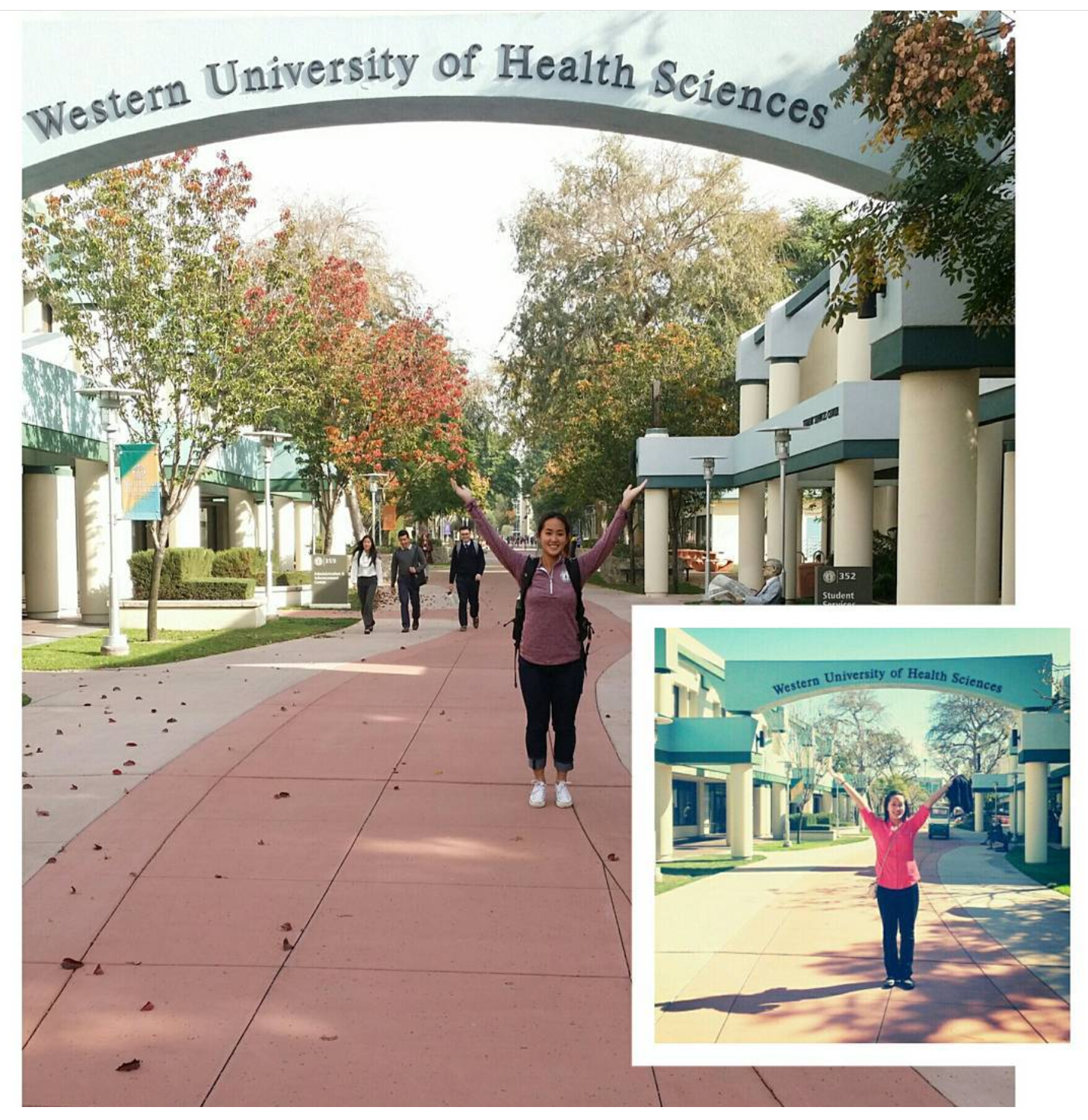 I was fortunate to have my last two affiliations back near home in Oregon. My PT program was located in Pomona, CA. My last day in Cali was a final and a celebration with my class (there may have been a party bus) and when I got home, I woke my husband up (around 3 am), took a 30-minute nap while he showered and we hit the road. 18-hour drive back to Oregon.
I was fortunate to have my last two affiliations back near home in Oregon. My PT program was located in Pomona, CA. My last day in Cali was a final and a celebration with my class (there may have been a party bus) and when I got home, I woke my husband up (around 3 am), took a 30-minute nap while he showered and we hit the road. 18-hour drive back to Oregon.